Half of fluid balance charts are never completed.
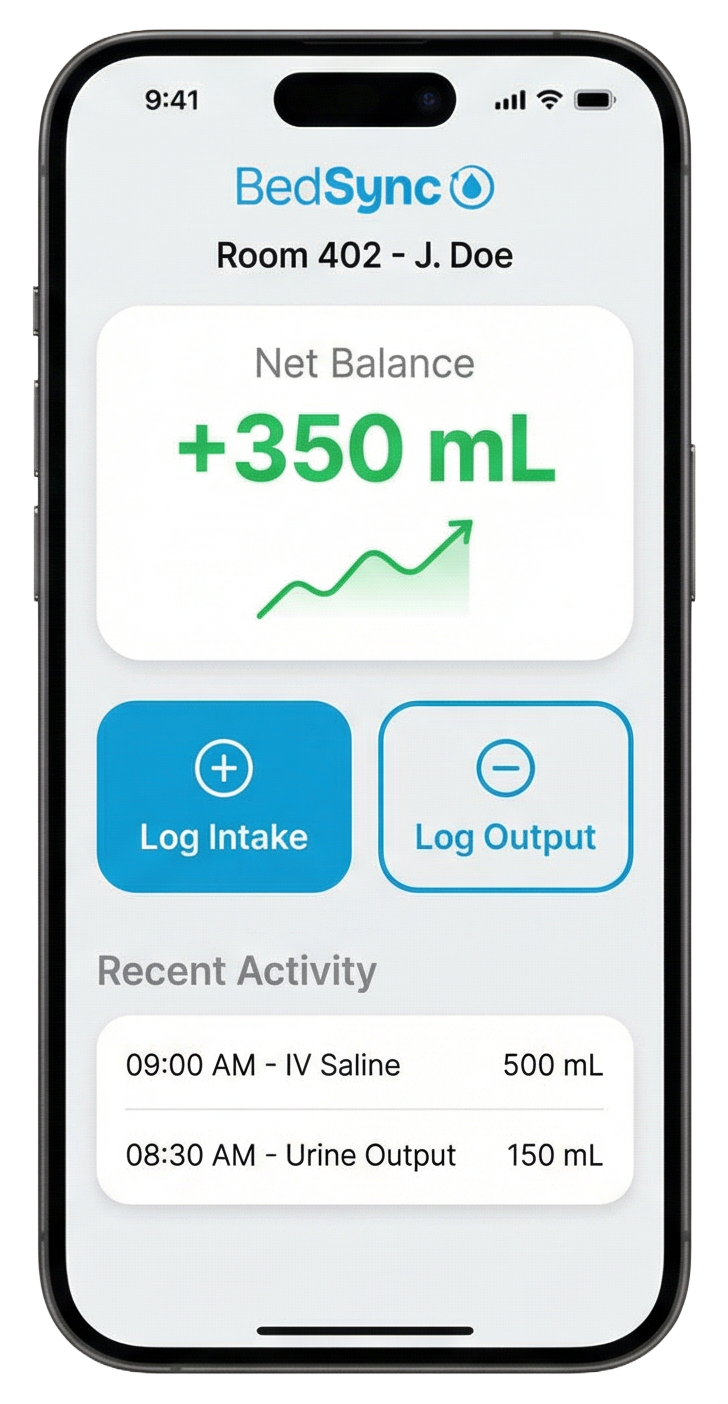
The ones that are? 25–35% contain calculation errors large enough to mask kidney injury—errors reaching up to 2,405 mL. Only 12% of patients ordered for I/O monitoring actually had documentation. BedSync replaces manual charting with voice and vision capture—speak it, scan it, sync it to the EHR.